Postpartum Depression (PPD): Understanding, Signs, and Support
Becoming a mother is a profound joy—but for many, the weeks after childbirth can bring intense emotional challenges. Postpartum Depression (PPD) is a major depressive condition that typically develops within the first year after delivery. Estimates suggest that over 1 in 5 new mothers in India experience significant postpartum stress. PPD is more serious than “baby blues.”
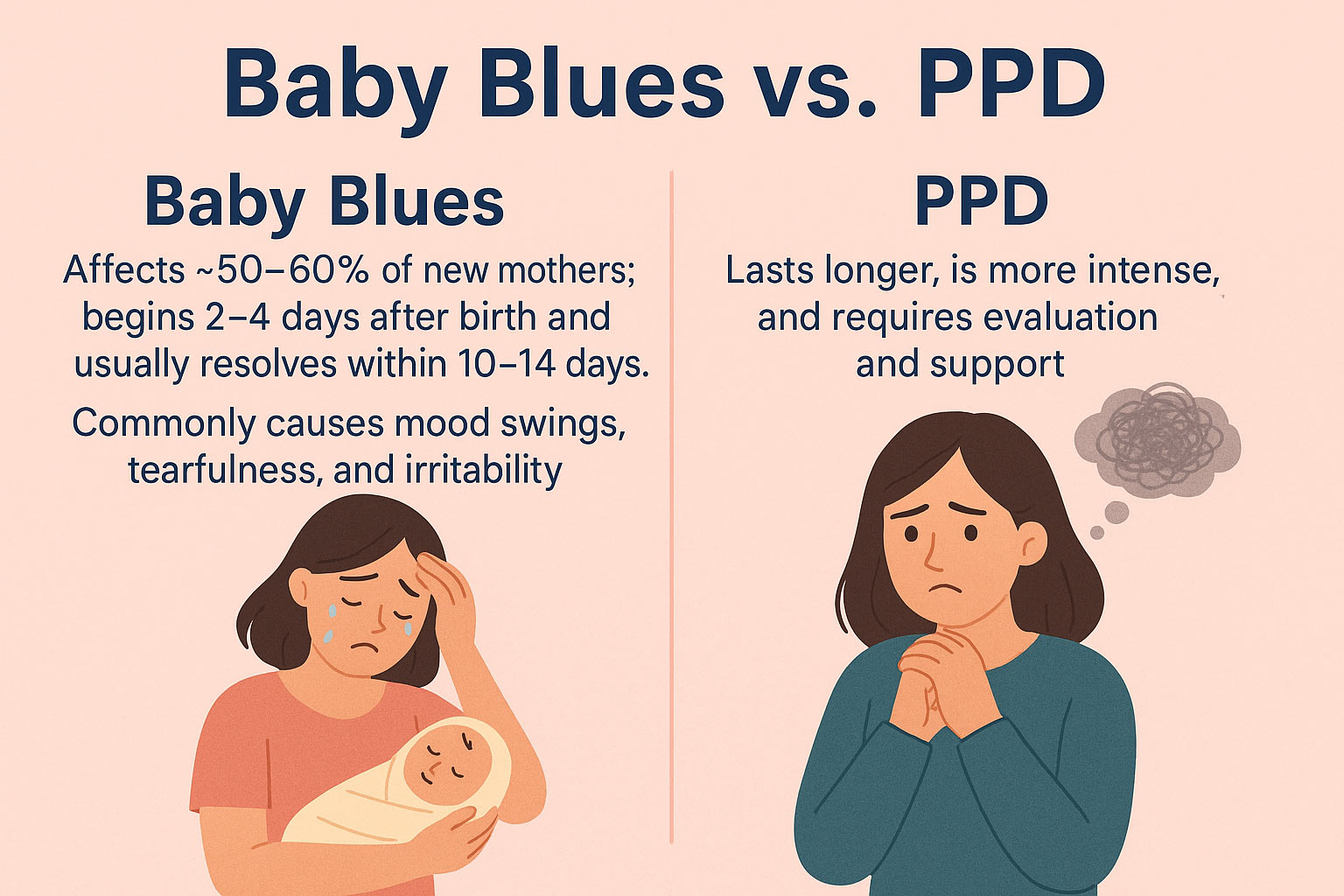
Baby Blues vs. PPD
-
Baby Blues: Affects ~50–60% of new mothers; begins 2–4 days after birth and usually resolves within 10–14 days. Commonly causes mood swings, tearfulness, and irritability.
-
PPD: Lasts longer, is more intense, and requires evaluation and support.
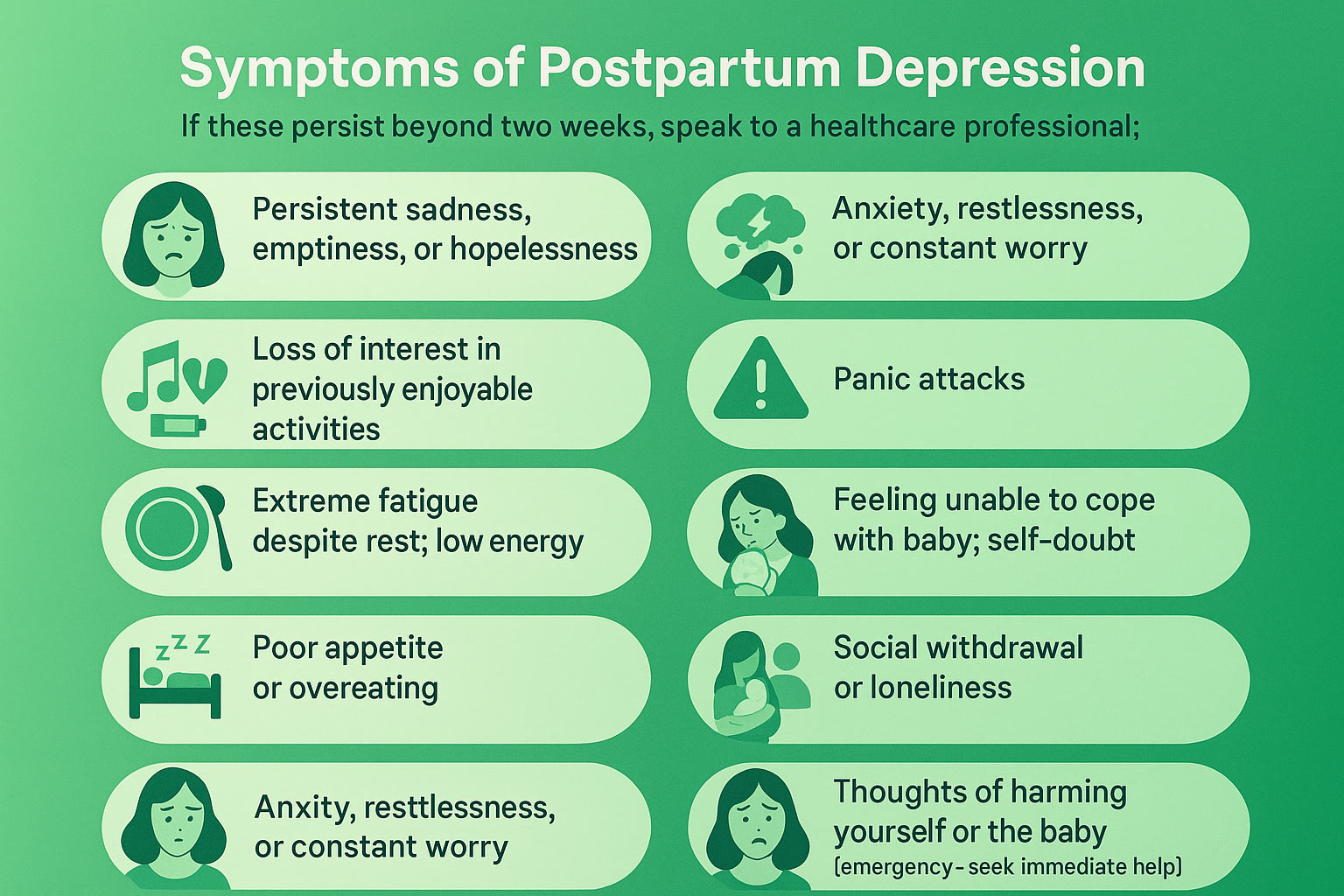
Symptoms of Postpartum Depression
If these persist beyond two weeks, speak to a healthcare professional:
-
Persistent sadness, emptiness, or hopelessness
-
Loss of interest in previously enjoyable activities
-
Extreme fatigue despite rest; low energy
-
Poor appetite or overeating
-
Sleep changes (insomnia or oversleeping)
-
Anxiety, restlessness, or constant worry
-
Panic attacks
-
Feeling unable to cope with baby; self-doubt
-
Social withdrawal or loneliness
-
Thoughts of harming yourself or the baby (emergency—seek immediate help)
Why Does PPD Happen?
PPD has no single cause—it’s a mix of biological, psychological, and social factors.
1) Biological/Hormonal
-
Rapid drop in estrogen and progesterone after birth can affect brain chemistry and mood
-
Thyroid changes may trigger depressive symptoms
-
Sleep deprivation disrupts emotional regulation
2) Psychological
-
Personal or family history of depression/anxiety
-
High worry during pregnancy (about baby’s or mother’s health)
-
Perfectionism and high self-pressure
3) Social
-
Lack of support from partner/family
-
Financial stress or single parenting
-
Baby or mother with medical complications
4) Lifestyle
-
Difficulty expressing needs or asking for help
-
Sudden change from active work/social life to home-bound routine, body image concerns, and loss of confidence
When to Seek Help (and From Whom)
-
If symptoms last more than 2 weeks, interfere with daily life, or if you have any thoughts of self-harm/harming the baby, seek help immediately.
-
Start with your obstetrician/gynecologist, family physician, or a mental health professional (psychologist/psychiatrist).
-
In emergencies, use local crisis services or go to the nearest hospital.
Evidence-Based Treatment Options
Treatment is individualized and safe plans can be made for breastfeeding mothers in consultation with clinicians.
-
Psychotherapy: Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT)
-
Medication: Antidepressants (e.g., SSRIs) when indicated by a physician
-
Support Groups & Peer Support: Sharing experiences reduces isolation
-
Address Medical Contributors: Check thyroid, anemia, sleep disorders
Practical Self-Care & Family Support
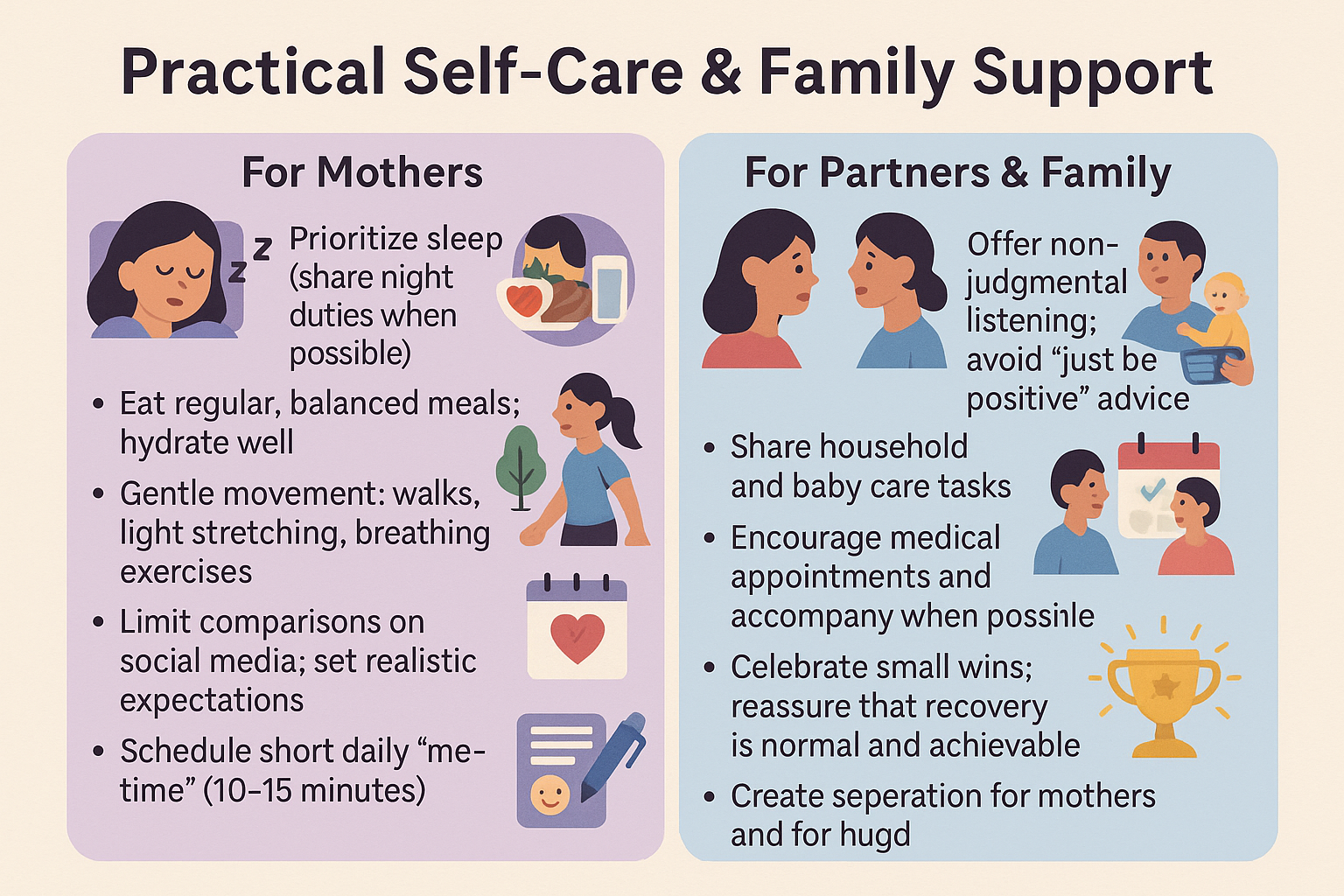
For Mothers
-
Prioritize sleep (share night duties when possible)
-
Eat regular, balanced meals; hydrate well
-
Gentle movement: walks, light stretching, breathing exercises
-
Limit comparisons on social media; set realistic expectations
-
Schedule short daily “me-time” (10–15 minutes)
-
Keep a symptom diary to track mood and triggers
For Partners & Family
-
Offer non-judgmental listening; avoid “just be positive” advice
-
Share household and baby care tasks
-
Encourage medical appointments and accompany when possible
-
Celebrate small wins; reassure that recovery is normal and achievable
Key Takeaway
PPD is common, real, and treatable. Early recognition, compassionate support, and professional care lead to recovery. Asking for help is a sign of strength—you are not alone.